Osteoarthritis of the Knee
Osteoarthritis of the knee happens when cartilage in your knee joint breaks down. When this happens, the bones in your knee joint rub together, causing friction that makes your knees hurt, become stiff or swell. Sometimes Osteoarthritis in the knee can’t be cured but there are treatments that can relieve symptoms and slow your condition’s progress.
Osteoarthritis (OA) of the knee is a common and debilitating joint disorder characterized by the gradual degradation of cartilage, which cushions the ends of the bones in the knee joint. This condition leads to pain, stiffness, and decreased function. Here’s a detailed overview:
Causes and Risk Factors
- Age: The risk of knee OA increases with age.
- Gender: Women are more likely to develop OA, particularly after age 50.
- Genetics: A family history of OA can increase the risk.
- Obesity: Excess weight puts additional stress on knee joints.
- Joint Injuries: Previous injuries to the knee can lead to OA.
- Repetitive Stress: Occupations or activities that put repetitive stress on the knee can contribute to OA.
- Bone Deformities: Congenital joint abnormalities or cartilage defects can lead to OA.
Symptoms
- Pain: Commonly worsens with activity and relieved by rest.
- Stiffness: Particularly after periods of inactivity or in the morning.
- Swelling: Due to inflammation in the joint.
- Loss of Flexibility: Difficulty moving the knee fully.
- Grinding Sensation: Feeling or hearing a grating sensation when using the knee.
- Bone Spurs: Extra bits of bone, which feel like hard lumps, may form around the knee joint.
Diagnosis
Diagnosis is typically based on a combination of:
- Medical History: Reviewing symptoms and any relevant history of knee injury.
- Physical Examination: Checking for tenderness, swelling, and range of motion.
- Imaging Tests: X-rays to show cartilage loss, bone damage, and bone spurs; MRI for detailed images of bone and soft tissues.
- Lab Tests: Analyzing joint fluid to rule out other types of arthritis.
Treatment
Treatment aims to manage symptoms and improve joint function. Options include:
Non-Pharmacological Treatments
- Weight Management: Reducing weight to decrease stress on the knee.
- Exercise: Strengthening the muscles around the knee and improving flexibility.
- Physical Therapy: Tailored exercises and treatments to improve knee function.
- Assistive Devices: Using braces, shoe inserts, or walking aids to relieve stress on the knee.
Pharmacological Treatments
- Pain Relievers: Acetaminophen or NSAIDs (e.g., ibuprofen).
- Topical Pain Relievers: Creams or ointments applied directly to the knee.
- Corticosteroid Injections: Reducing inflammation and pain.
- Hyaluronic Acid Injections: Supplementing the joint fluid to improve mobility.
Surgical Options
- Arthroscopy: Removing loose fragments of bone or cartilage.
- Osteotomy: Realigning the knee to relieve pressure on the joint.
- Joint Replacement: Partial or total knee replacement in severe cases.
Prevention
While OA cannot be completely prevented, certain measures can reduce the risk:
- Maintain a Healthy Weight: Reducing stress on the knee joints.
- Stay Active: Regular exercise to strengthen muscles around the knee.
- Avoid Joint Injuries: Using proper techniques during physical activities.
- Healthy Diet: Ensuring adequate intake of nutrients that support joint health, like Vitamin D and calcium.
Surgical Options
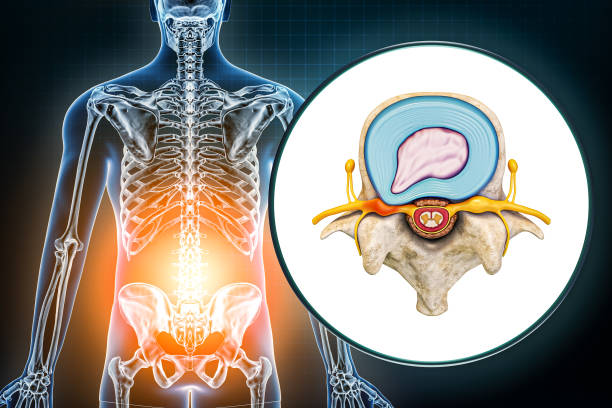
The lumbar spine is the lower back portion of the spine, consisting of five vertebrae labeled L1 to L5. These vertebrae are the largest in the spine, and they provide support for the upper body and protect the spinal cord.
Intervertebral discs are located between each pair of adjacent vertebrae. The discs are composed of a tough outer layer called the annulus fibrosus and a soft, gel-like inner core called the nucleus pulposus. The function of the intervertebral discs is to act as shock absorbers for the spine, allowing for movement and flexibility.
The outer fibrous ring is composed of fibrocartilage and surrounds the nucleus pulposus, holding it in place. The nucleus pulposus is composed of water, collagen, and proteoglycans, which provide it with its elasticity and compressibility. Together, the annulus fibrosus and the nucleus pulposus allow for spinal movement while providing support and stability to the spine.
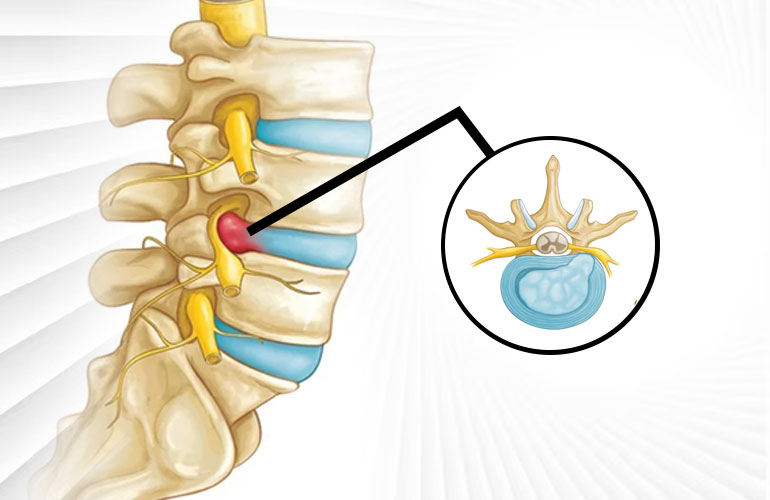
Causes and PLID Meaning
The primary cause of prolapsed lumbar intervertebral disc (PLID) is the degeneration of the lumbar disc herniation due to aging. As we age, the water content of the nucleus pulposus decreases, making it less elastic and more susceptible to injury. This can cause the disc to become brittle and prone to cracking or tearing, leading to prolapse.
Other Causes of PLID Include:
- Trauma or injury to the back, such as a fall or car accident
- Repetitive lifting or twisting motions
- Obesity or excess weight, which puts increased stress on the lumbar spine
- Poor posture or spinal alignment, which can place undue stress on the lower back and increase the risk of disc injury.
It is important to note that not everyone with these risk factors will develop PLID, and some people with no risk factors may still develop the condition. However, being aware of these risk factors can help individuals take steps to reduce the risk of future of developing PLID.
PLID Symptoms and Diagnosis
Symptoms of PLID can vary depending on the severity and location of the lumbar disc prolapsed, but they often include:
- Lower back pain
- Radiating pain down the legs, commonly referred to as sciatica/li>
- Numbness or tingling in the legs or feet
- Muscle weakness or difficulty moving the legs
- Loss of bladder or bowel control in severe cases.
Diagnosis of PLID
Diagnosis of PLID typically involves a physical exam, medical history, or clinical examination and diagnostic tests. The physical exam may include testing reflexes, checking muscle strength, and assessing sensation in the leg raise test. The medical history may include questions about the duration and severity of symptoms, history of trauma, as well as any risk factors, or previous injuries.